Bone Grafts and Substitutes in Orthopedic Surgery - An Overview
What is a bone graft?
Bone grafting is a surgical procedure to repair or rebuild damaged or diseased bones with the help of transplanted bone tissue or a similar synthetic material. Traditionally, bone graft surgery relied on autogenous bone grafts, or bone tissue extracted from other parts of the patient’s body. However, due to the limitations of autografts, modern bone graft surgeries often deploy synthetic bone substitutes instead.
Given the growing prevalence of orthopedic diseases that require surgical intervention, the demand for bone graft substitutes is also rising. According to a recent market report, the global bone graft substitutes market was valued at USD 3 billion in 2023 and is expected to expand at 6.6% CAGR from 2024 to 2032 [1].
In this blog post, we shall compare the properties of different types of bone grafts and identify the characteristics of ideal bone graft substitutes, as listed in scientific literature.
Types of Bone Grafts
Bone grafts can be classified into three categories based on the source they are derived from and each of these offers a unique set of advantages and limitations.
-
Autogenous Bone Grafts or Autografts
Autografts involve the transplantation of bone tissue from one part of a patient’s body to another. The most common donor sites for autografts include the iliac crest (pelvic bone), ribs, and fibula (lower leg bone). Autografts are still considered the gold standard for orthopedic surgery by many as they provide live bone cells and a natural scaffold for bone regeneration, promoting successful integration. Furthermore, since the bone tissue is obtained from the patient itself, the chances of rejection are minimized. However, autografts require an additional surgery for extraction, and are often prone to bone harvesting complications.
-
Allografts
Allografts involve the use of bone tissue from a human donor. They can be used as a substitute for an autograft when there is a limited supply of the patient’s own bone or when a larger bone graft is needed. These grafts are processed and sterilized to reduce the risk of rejection. They offer better ease of use, diversity in shapes and sizes, and reduced surgical complications compared to autografts. However, the limited availability of donors may not be able to meet the growing demand for allografts, which is why synthetic bone graft substitutes are the need of the hour.
-
Synthetic Bone Substitutes
Synthetic bone substitutes are man-made materials that are designed to mimic the natural properties of bone. They can be synthesized using different materials such as ceramics, bioactive glasses, polymers, or composites. The ease of availability and sterilization of commercially available synthetic bone substitutes is often offset by less-than-ideal mechanical or biological properties, making them suitable for specific clinical applications but unsuited for others.
Given the unique advantages and limitations of each type of bone graft, the choice of bone graft is usually governed by factors such as availability, the size of the defect, the patient’s health, and the surgeon’s preference.
Properties of an Ideal Bone Graft
The suitability of bone grafts for orthopedic surgery is usually evaluated on parameters such as 1) ability to support new bone formation – osteoconduction 2) mechanical properties and 3) resorption rate. All bone grafts must display the ability of cells or tissues to generate or promote the formation of bone. Osteoconduction involves the provision of a 3D scaffold for bone cells from neighboring tissue to attach, multiply, differentiate and deposit new bone. Additionally, an ideal bone graft should have similar mechanical properties as bone and must offer optimal support at the graft site. Furthermore, the resorption rate or the rate of degradation of the graft should match the rate of new bone formation.
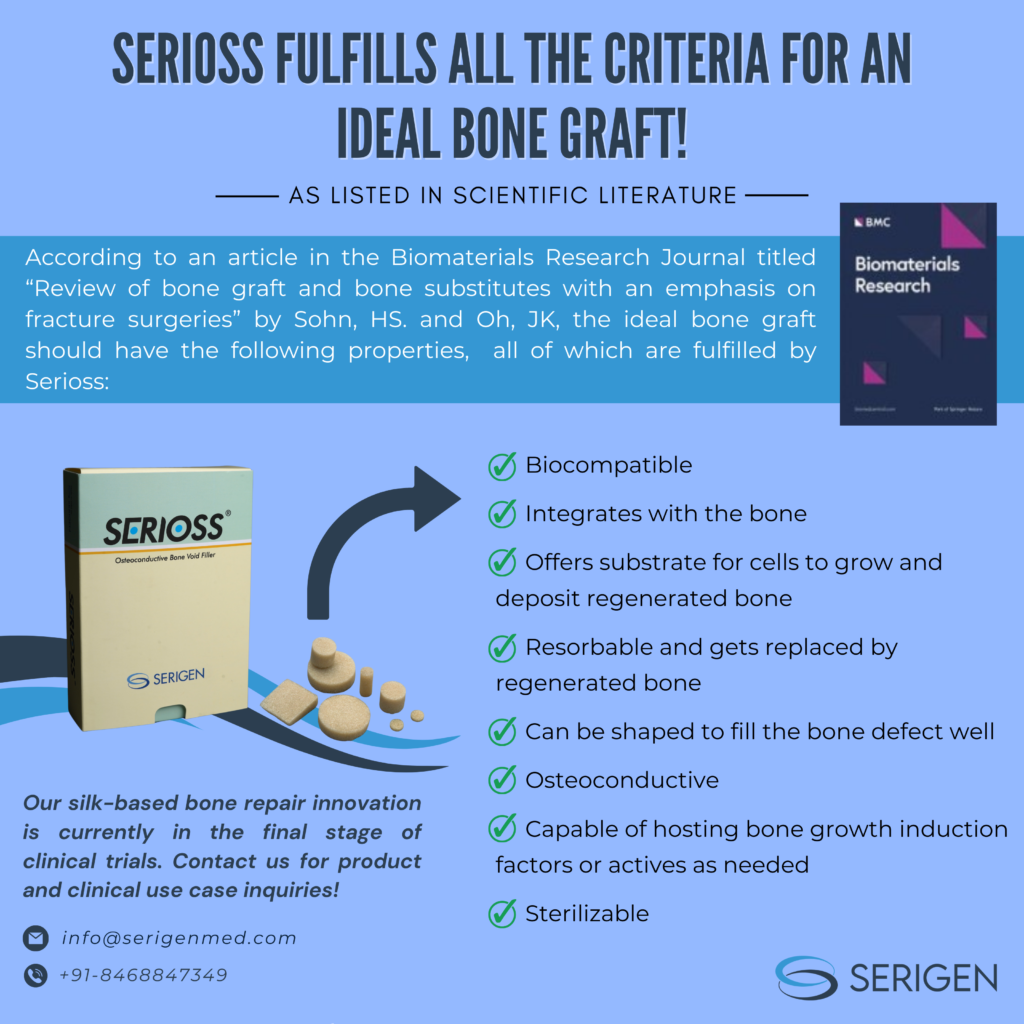
According to an article in the Biomaterials Research Journal titled “Review of bone graft and bone substitutes with an emphasis on fracture surgeries” by Sohn, HS. and Oh, JK [2], most commercially available bone graft substitutes fall short on at least one of the desired parameters, limiting their clinical applications. The article further states that the ideal bone graft should have the following properties:
- Biocompatible
- Integrates with the bone
- Offers substrate for cells to grow and deposit regenerated bone
- Resorbable and gets replaced by regenerated bone
- Can be shaped to fill the bone defect well
- Osteoconductive
- Capable of hosting bone growth induction factors or actives as needed
- Sterilizable
At Serigen we use our patented technology for the fabrication of Serioss, a silk-based scaffold for bone tissue regeneration that fulfills all the above criteria for an ideal bone graft!
Serioss is a silk-based bone void filler, suitable for a wide range of clinical use cases that demand bone tissue regeneration, such as trauma, infection, or cancer. It has optimum bulk porosity with an interconnected pore architecture that provides a 3D scaffold for cells to ingress, adhere, interact, proliferate and differentiate. Furthermore, Serioss has mechanical properties equivalent to that of native cancellous bone, is osteoconductive, and supports the differentiation of bone cells in vitro and in vivo. In animal and lab studies, Serioss has exhibited 2x better bone repair than leading ceramic-based bone void fillers, making it a promising alternative to existing bone graft substitutes.
Conclusion
With the growing need for bone graft surgeries, synthetic bone graft substitutes are becoming the bone graft of choice, given the surgical complications associated with autografts and the limited availability of allografts. However, commercially available synthetic bone graft substitutes may not be suitable for all orthopedic surgeries as they often have a few suboptimal characteristics in terms of bone formation capabilities, resorption rate or mechanical properties.
Serioss is an osteoconductive bone void filler powered by silk protein that addresses this gap by combining the performance of an autograft with the convenience of silk biomaterials. Furthermore, it fulfills all the criteria of an ideal bone graft, as listed in scientific literature. Therefore, Serioss can serve as a revolutionary 3D scaffold for bone tissue regeneration!
With promising results from ongoing clinical trials, Serioss is one step away from being launched in the market, to address the unmet need for a high-performing synthetic bone graft for orthopedic surgeries.
References
- https://www.gminsights.com/industry-analysis/bone-graft-substitutes-market
- https://biomaterialsres.biomedcentral.com/articles/10.1186/s40824-019-0157-y

Author Bio – Dr Premnath Venugopalan is Co-founder and Chair at Serigen Mediproducts. He holds a PhD from MIT USA and is a trained chemical engineer from IIT-Bombay (Distinguished Alumnus, 2022), along with being a Chevening Technology Enterprise Scholar in Cambridge, UK. He is also Head, NCL Innovations at CSIR-NCL and Founder Director at Venture Center.
What is a bone graft?
Bone grafting is a surgical procedure to repair or rebuild damaged or diseased bones with the help of transplanted bone tissue or a similar synthetic material. Traditionally, bone graft surgery relied on autogenous bone grafts, or bone tissue extracted from other parts of the patient’s body. However, due to the limitations of autografts, modern bone graft surgeries often deploy synthetic bone substitutes instead.
Given the growing prevalence of orthopedic diseases that require surgical intervention, the demand for bone graft substitutes is also rising. According to a recent market report, the global bone graft substitutes market was valued at USD 3 billion in 2023 and is expected to expand at 6.6% CAGR from 2024 to 2032 [1].
In this blog post, we shall compare the properties of different types of bone grafts and identify the characteristics of ideal bone graft substitutes, as listed in scientific literature.
Types of Bone Grafts
Bone grafts can be classified into three categories based on the source they are derived from and each of these offers a unique set of advantages and limitations.
-
Autogenous Bone Grafts or Autografts
Autografts involve the transplantation of bone tissue from one part of a patient’s body to another. The most common donor sites for autografts include the iliac crest (pelvic bone), ribs, and fibula (lower leg bone). Autografts are still considered the gold standard for orthopedic surgery by many as they provide live bone cells and a natural scaffold for bone regeneration, promoting successful integration. Furthermore, since the bone tissue is obtained from the patient itself, the chances of rejection are minimized. However, autografts require an additional surgery for extraction, and are often prone to bone harvesting complications.
-
Allografts
Allografts involve the use of bone tissue from a human donor. They can be used as a substitute for an autograft when there is a limited supply of the patient’s own bone or when a larger bone graft is needed. These grafts are processed and sterilized to reduce the risk of rejection. They offer better ease of use, diversity in shapes and sizes, and reduced surgical complications compared to autografts. However, the limited availability of donors may not be able to meet the growing demand for allografts, which is why synthetic bone graft substitutes are the need of the hour.
-
Synthetic Bone Substitutes
Synthetic bone substitutes are man-made materials that are designed to mimic the natural properties of bone. They can be synthesized using different materials such as ceramics, bioactive glasses, polymers, or composites. The ease of availability and sterilization of commercially available synthetic bone substitutes is often offset by less-than-ideal mechanical or biological properties, making them suitable for specific clinical applications but unsuited for others.
Given the unique advantages and limitations of each type of bone graft, the choice of bone graft is usually governed by factors such as availability, the size of the defect, the patient’s health, and the surgeon’s preference.
Properties of an Ideal Bone Graft
The suitability of bone grafts for orthopedic surgery is usually evaluated on parameters such as 1) ability to support new bone formation – osteoconduction 2) mechanical properties and 3) resorption rate. All bone grafts must display the ability of cells or tissues to generate or promote the formation of bone. Osteoconduction involves the provision of a 3D scaffold for bone cells from neighboring tissue to attach, multiply, differentiate and deposit new bone. Additionally, an ideal bone graft should have similar mechanical properties as bone and must offer optimal support at the graft site. Furthermore, the resorption rate or the rate of degradation of the graft should match the rate of new bone formation.
According to an article in the Biomaterials Research Journal titled “Review of bone graft and bone substitutes with an emphasis on fracture surgeries” by Sohn, HS. and Oh, JK [2], most commercially available bone graft substitutes fall short on at least one of the desired parameters, limiting their clinical applications. The article further states that the ideal bone graft should have the following properties:
- Biocompatible
- Integrates with the bone
- Offers substrate for cells to grow and deposit regenerated bone
- Resorbable and gets replaced by regenerated bone
- Can be shaped to fill the bone defect well
- Osteoconductive
- Capable of hosting bone growth induction factors or actives as needed
- Sterilizable
At Serigen we use our patented technology for the fabrication of Serioss, a silk-based scaffold for bone tissue regeneration that fulfills all the above criteria for an ideal bone graft!
Serioss is a silk-based bone void filler, suitable for a wide range of clinical use cases that demand bone tissue regeneration, such as trauma, infection, or cancer. It has optimum bulk porosity with an interconnected pore architecture that provides a 3D scaffold for cells to ingress, adhere, interact, proliferate and differentiate. Furthermore, Serioss has mechanical properties equivalent to that of native cancellous bone, is osteoconductive, and supports the differentiation of bone cells in vitro and in vivo. In animal and lab studies, Serioss has exhibited 2x better bone repair than leading ceramic-based bone void fillers, making it a promising alternative to existing bone graft substitutes.
Conclusion
With the growing need for bone graft surgeries, synthetic bone graft substitutes are becoming the bone graft of choice, given the surgical complications associated with autografts and the limited availability of allografts. However, commercially available synthetic bone graft substitutes may not be suitable for all orthopedic surgeries as they often have a few suboptimal characteristics in terms of bone formation capabilities, resorption rate or mechanical properties.
Serioss is an osteoconductive bone void filler powered by silk protein that addresses this gap by combining the performance of an autograft with the convenience of silk biomaterials. Furthermore, it fulfills all the criteria of an ideal bone graft, as listed in scientific literature.
Therefore, Serioss can serve as a revolutionary 3D scaffold for bone tissue regeneration!
With promising results from ongoing clinical trials, Serioss is one step away from being launched in the market, to address the unmet need for a high-performing synthetic bone graft for orthopedic surgeries.
References
- https://www.gminsights.com/industry-analysis/bone-graft-substitutes-market
- https://biomaterialsres.biomedcentral.com/articles/10.1186/s40824-019-0157-y

Author Bio – Dr Premnath Venugopalan is Co-founder and Chair at Serigen Mediproducts. He holds a PhD from MIT USA and is a trained chemical engineer from IIT-Bombay (Distinguished Alumnus, 2022), along with being a Chevening Technology Enterprise Scholar in Cambridge, UK. He is also Head, NCL Innovations at CSIR-NCL and Founder Director at Venture Center.