Tissue Engineering In Orthopaedics – Latest Advancements
What is the significance of tissue engineering in regenerative medicine?
Regenerative medicine is a branch of medicine that investigates techniques to replace or regenerate cells, tissues, or organs to restore their normal function [1]. Regeneration of damaged tissues/organs is an active field of research under regenerative medicine. Tissues have limited self-regeneration capacity against damage to tissues that can be caused by trauma, disease, and aging. When the damage is beyond the self-repair ability of the tissue, it needs assistance for repair. This is where tissue engineering comes into the picture. Tissue engineering can be used for both soft and hard tissue regeneration. The tissue engineering approach involves the use of a scaffolding material that provides appropriate cues for the cells and tissues to regenerate. Different natural and synthetic biomaterials have been explored as scaffolding materials for skin, nerve, and artificial blood vessel regeneration, bone regeneration, etc. Hence, tissue engineering plays a crucial role in tissue/organ repair and regeneration.
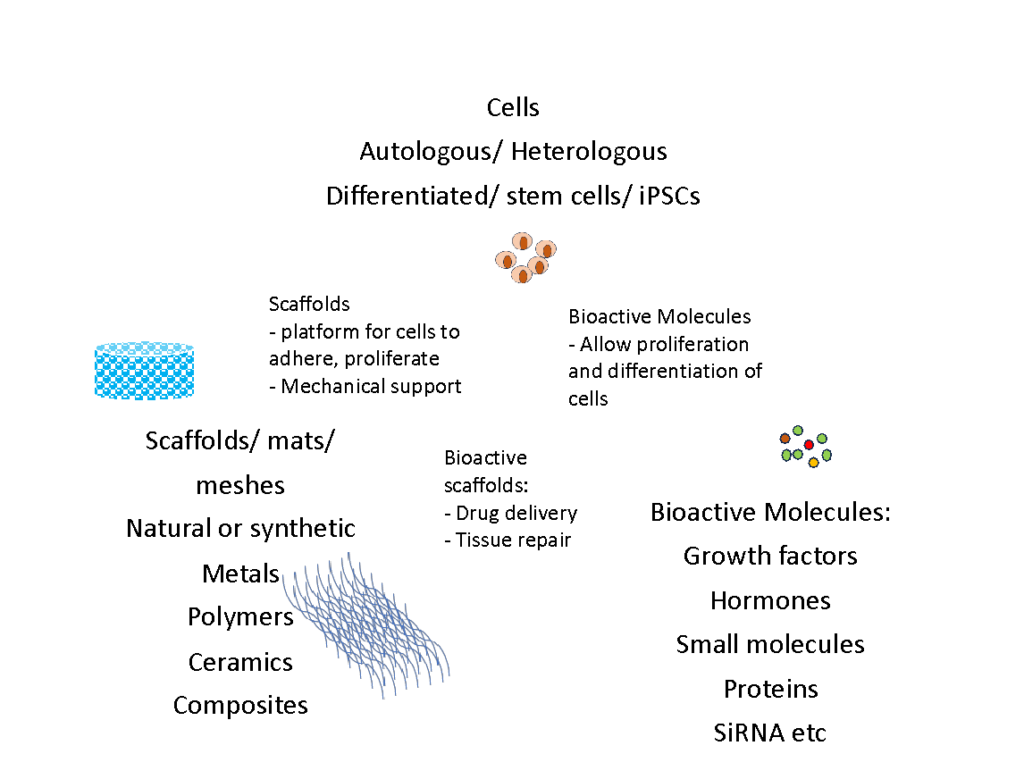
Strategies for Tissue Engineering
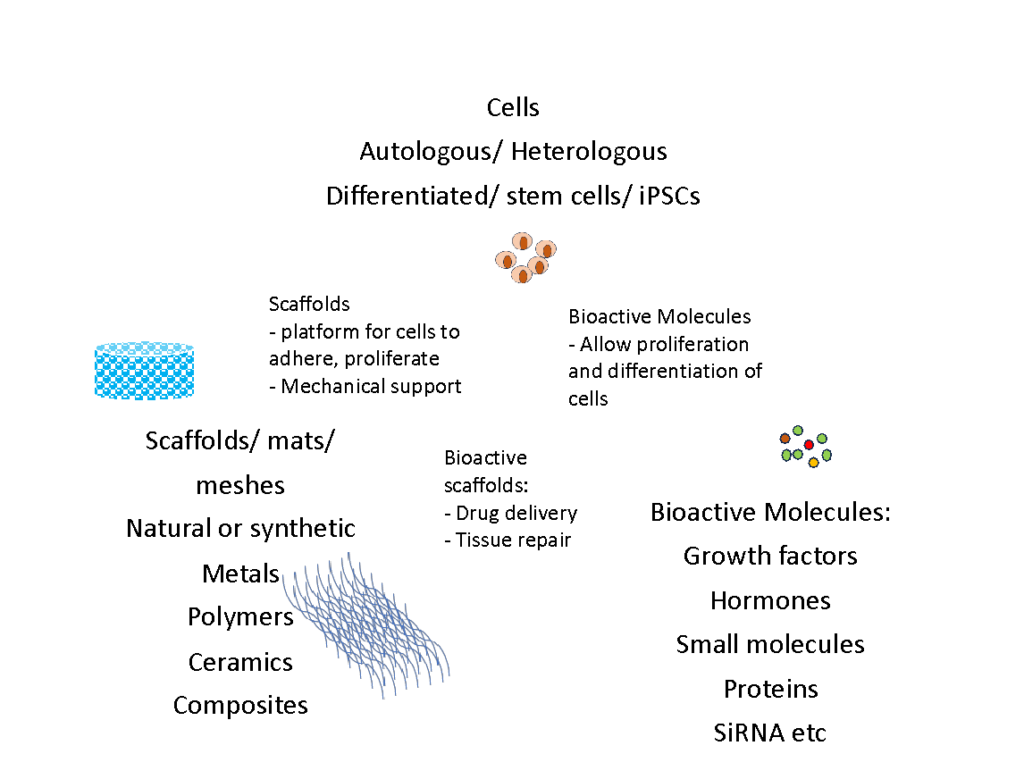
Tissue engineering involves the association of healthy cells, biomaterials and active factors to repair the damage. These three elements of tissue engineering can be used independently or in combination to generate tissues in numerous ways. Scaffolds made using natural or synthetic materials are an essential component of tissue engineering as they activate the surrounding tissue cells via mechanical and/or chemical cues. They can be used with or without seeding cells externally. When seeded with cells, they hold the cells at the injury site. When used without the cells, they provide the platform for cells to adhere, proliferate and differentiate in order to restore and improve tissue function.
Applications of Tissue Engineering In Orthopaedics
Bone defects are caused by fractures, bone disease, bone infections and tumour resection. Regeneration and repair of the damaged bone presents significant challenges in the field of regenerative medicine. Tissue engineering is a promising approach to address clinical needs for bone regeneration and repair. Tissue engineering in orthopaedics mainly aims at the development of 3D scaffolds, which provide the structural support for new bone formation [1]. Various synthetic and natural materials have been explored in bone tissue engineering. The ideal scaffold for bone tissue engineering applications should be porous with interconnected porosity, biocompatible, osteoconductive/osteoinductive, and should provide surface parameters suitable for cell attachment, proliferation and differentiation. It should also mimic the mechanical properties of native bone. Ceramic-based scaffolds are the most common among all the materials used for bone tissue engineering. Though used extensively, they show poor osteointegration and impose the risk of secondary fractures, ultimately resulting in poor-quality bone formation [2],[3].
What are osteoinduction, osteoconduction and osseointegration?
As mentioned above, bone scaffolding materials should be either osteoconductive and/or osteoinductive. Osteoinduction is a process that stimulates bone formation by the recruitment of immature (undifferentiated/stem cells) cells at the site of implantation. With proper cues, these cells undergo differentiation into mature osteoblasts (bone cells). Osteoinductive materials are “smart materials” as they allow ectopic bone formation by providing cues essential for bone formation. On the other hand, osteoconduction is a process in which bone cells attach to the implant surface and initiate bone formation, vascularization and new blood vessel formation. Osteointegration refers to the establishment of a structural and functional connection between the old bone and the new bone. During osteointegration, the implant becomes an integral part of the bone. 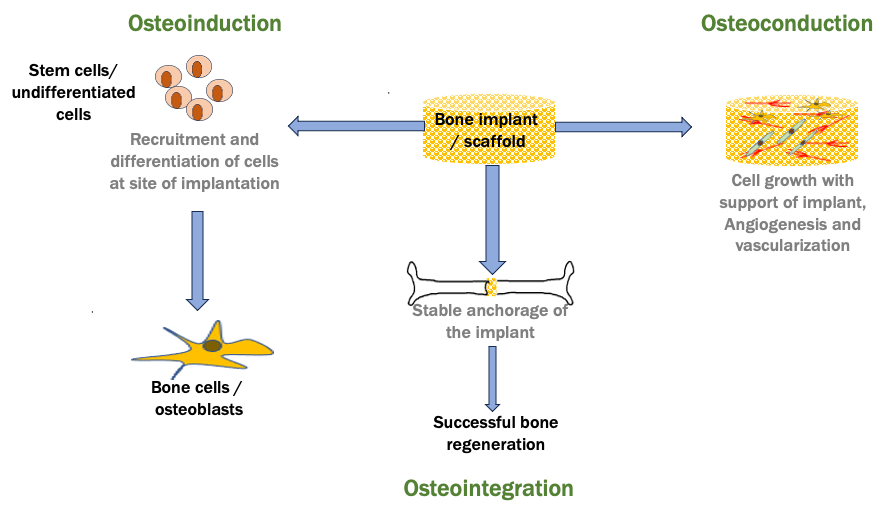
Serigen’s contribution to cutting-edge tissue engineering for orthopaedics
Silk is a natural protein polymer that has gained attention in the field of tissue engineering due to its biocompatibility, ease of availability and ease of processability. Serigen has developed silk-based products for hard and soft tissue regeneration and for advanced wound care. One of our inventions – Serioss, a silk-based bone void filler – is a revolutionary product in the field of bone tissue engineering.
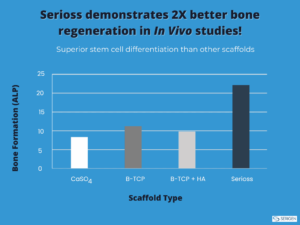
Serioss has optimum bulk porosity with interconnected pore architecture, which provides the platform for cells to ingress, adhere, interact, proliferate and differentiate. It has mechanical properties equivalent to that of native cancellous bone [2],[3]. Furthermore, Serioss is osteoconductive in nature and supports the differentiation of bone cells in vitro and in vivo. After successfully completing the world’s first clinical for the use of silk biomaterials in bone repair, Serioss is currently undergoing stage 2 pivotal clinical trials.
Conclusion
Tissue engineering using biomaterials is the future of treatment for orthopaedic pathology. In these applications, silk is a promising biopolymer for hard and soft tissue engineering owing to its unique properties. With its groundbreaking research in the field of silk-based tissue engineering solutions for bone repair, Serigen is paving the path for superior bone healing through tissue engineering using silk!
References
1. Tatara AM, Mikos AG. Tissue Engineering in Orthopaedics. J Bone Joint Surg Am. 2016 Jul 6;98(13):1132-9. doi: 10.2106/JBJS.16.00299. PMID: 27385687; PMCID: PMC4928040.
2. Deshpande R, Shukla S, Kale A, Deshmukh N, Nisal A, Venugopalan P. Silk Fibroin Microparticle Scaffold for Use in Bone Void Filling: Safety and Efficacy StudiesACS Biomater. Sci. Eng. 2022, 8, 3, 1226–1238

Author Bio – Rucha Deshpande is Manager R&D at Serigen Mediproducts. She holds a PhD in Zoology from the University of Pune and has 7 years of professional experience in tissue engineering, cell culture and molecular biology.
What is the significance of tissue engineering in regenerative medicine?
Regenerative medicine is a branch of medicine that investigates techniques to replace or regenerate cells, tissues, or organs to restore their normal function [1]. Regeneration of damaged tissues/organs is an active field of research under regenerative medicine. Tissues have limited self-regeneration capacity against damage to tissues that can be caused by trauma, disease, and aging. When the damage is beyond the self-repair ability of the tissue, it needs assistance for repair. This is where tissue engineering comes into the picture. Tissue engineering can be used for both soft and hard tissue regeneration. The tissue engineering approach involves the use of a scaffolding material that provides appropriate cues for the cells and tissues to regenerate. Different natural and synthetic biomaterials have been explored as scaffolding materials for skin, nerve, and artificial blood vessel regeneration, bone regeneration, etc. Hence, tissue engineering plays a crucial role in tissue/organ repair and regeneration.
Strategies for Tissue Engineering
Tissue engineering involves the association of healthy cells, biomaterials and active factors to repair the damage. These three elements of tissue engineering can be used independently or in combination to generate tissues in numerous ways. Scaffolds made using natural or synthetic materials are an essential component of tissue engineering as they activate the surrounding tissue cells via mechanical and/or chemical cues. They can be used with or without seeding cells externally. When seeded with cells, they hold the cells at the injury site. When used without the cells, they provide the platform for cells to adhere, proliferate and differentiate in order to restore and improve tissue function.
Applications of Tissue Engineering In Orthopaedics
Bone defects are caused by fractures, bone disease, bone infections and tumour resection. Regeneration and repair of the damaged bone presents significant challenges in the field of regenerative medicine. Tissue engineering is a promising approach to address clinical needs for bone regeneration and repair. Tissue engineering in orthopaedics mainly aims at the development of 3D scaffolds, which provide the structural support for new bone formation [1]. Various synthetic and natural materials have been explored in bone tissue engineering. The ideal scaffold for bone tissue engineering applications should be porous with interconnected porosity, biocompatible, osteoconductive/osteoinductive, and should provide surface parameters suitable for cell attachment, proliferation and differentiation. It should also mimic the mechanical properties of native bone. Ceramic-based scaffolds are the most common among all the materials used for bone tissue engineering. Though used extensively, they show poor osteointegration and impose the risk of secondary fractures, ultimately resulting in poor-quality bone formation [2],[3].
What are osteoinduction, osteoconduction and osseointegration?
As mentioned above, bone scaffolding materials should be either osteoconductive and/or osteoinductive. Osteoinduction is a process that stimulates bone formation by the recruitment of immature (undifferentiated/stem cells) cells at the site of implantation. With proper cues, these cells undergo differentiation into mature osteoblasts (bone cells). Osteoinductive materials are “smart materials” as they allow ectopic bone formation by providing cues essential for bone formation. On the other hand, osteoconduction is a process in which bone cells attach to the implant surface and initiate bone formation, vascularization and new blood vessel formation. Osteointegration refers to the establishment of a structural and functional connection between the old bone and the new bone. During osteointegration, the implant becomes an integral part of the bone. 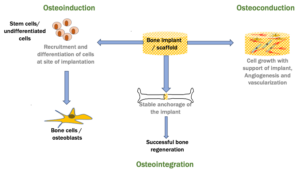
Serigen’s contribution to cutting-edge tissue engineering for orthopaedics
Silk is a natural protein polymer that has gained attention in the field of tissue engineering due to its biocompatibility, ease of availability and ease of processability. Serigen has developed silk-based products for hard and soft tissue regeneration and for advanced wound care. One of our inventions – Serioss, a silk-based bone void filler – is a revolutionary product in the field of bone tissue engineering.
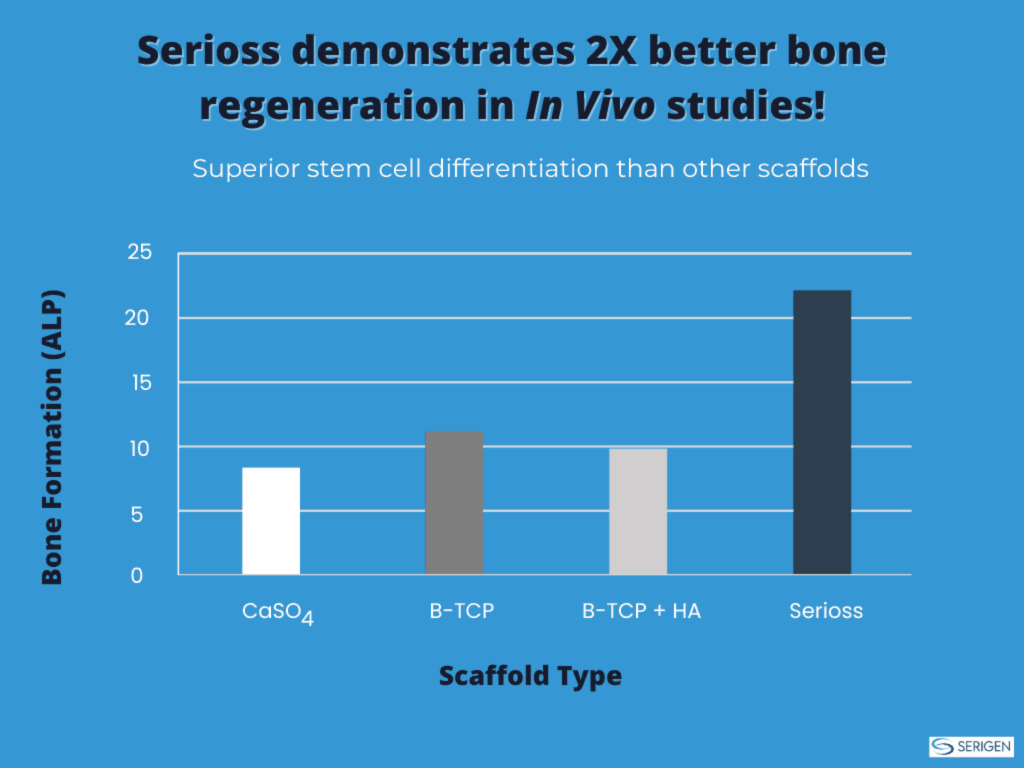
Serioss has optimum bulk porosity with interconnected pore architecture, which provides the platform for cells to ingress, adhere, interact, proliferate and differentiate. It has mechanical properties equivalent to that of native cancellous bone [2],[3]. Furthermore, Serioss is osteoconductive in nature and supports the differentiation of bone cells in vitro and in vivo. After successfully completing the world’s first clinical for the use of silk biomaterials in bone repair, Serioss is currently undergoing stage 2 pivotal clinical trials.
Conclusion
Tissue engineering using biomaterials is the future of treatment for orthopaedic pathology. In these applications, silk is a promising biopolymer for hard and soft tissue engineering owing to its unique properties. With its groundbreaking research in the field of silk-based tissue engineering solutions for bone repair, Serigen is paving the path for superior bone healing through tissue engineering using silk!
References
1. Tatara AM, Mikos AG. Tissue Engineering in Orthopaedics. J Bone Joint Surg Am. 2016 Jul 6;98(13):1132-9. doi: 10.2106/JBJS.16.00299. PMID: 27385687; PMCID: PMC4928040.
2. Deshpande R, Shukla S, Kale A, Deshmukh N, Nisal A, Venugopalan P. Silk Fibroin Microparticle Scaffold for Use in Bone Void Filling: Safety and Efficacy StudiesACS Biomater. Sci. Eng. 2022, 8, 3, 1226–1238

Author Bio – Rucha Deshpande is Manager R&D at Serigen Mediproducts. She holds a PhD in Zoology from the University of Pune and has 7 years of professional experience in tissue engineering, cell culture and molecular biology.